What is Sleep Apnea? Understanding This Common Sleep Disorder and How It Affects Your Health
Table of Contents
Introduction
You know that feeling when you wake up after supposedly sleeping for eight hours, but you feel like you’ve been hit by a truck? Yeah, I lived with that for almost five years before I figured out what was actually going on.
Here’s a crazy stat that made my jaw drop: roughly 39 million adults in the United States have sleep apnea, but a huge chunk of them have no clue they’re dealing with it. I was one of those people, stumbling through life exhausted, cranky, and wondatering why three cups of coffee didn’t even make a dent in my fatigue anymore. So th
Sleep apnea is basically when your breathing repeatedly stops and starts while you’re sleeping, and it’s way more serious than just annoying snoring. We’re talking about a condition that can mess with your heart, your brain, your mood, and pretty much every aspect of your daily life. But here’s the good news—once you understand what’s happening and get the right treatment, it’s like someone turned the lights back on in your life.
I’m gonna walk you through everything I wish someone had told me years ago about sleep apnea, from what it actually is to how you can tell if you’ve got it and what you can do about it.
It’s important to understand what is sleep apnea, as it can have significant effects on your health if left untreated.
Understanding Sleep Apnea: The Basics
Alright, let’s break this down in plain English. Sleep apnea happens when your breathing gets interrupted during sleep—sometimes for just a few seconds, sometimes for way longer. And we’re not talking about just one or two times a night, either.
When I finally got diagnosed, the sleep doctor told me I was stopping breathing around 47 times per hour. Forty-seven times! My wife had been complaining about my snoring for years, but I just thought, “Hey, I’m a middle-aged dude, that’s what we do.” Turns out, those dramatic gasping sounds she described weren’t just normal snoring—they were my body literally fighting to breathe again after each pause.
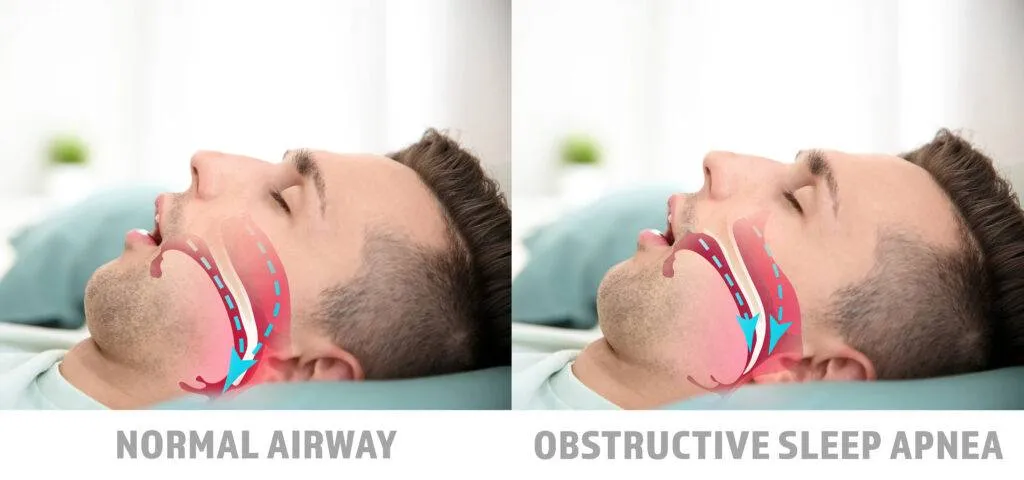
Here’s what’s happening in your body during these episodes. Your airway either gets blocked (like a clogged pipe) or your brain forgets to send the signal to breathe (which is arguably even weirder). Each time it happens, your oxygen levels drop, and your brain has to partially wake you up to restart your breathing.
The kicker? You usually don’t remember these wake-ups at all. You might think you slept through the night, but really your sleep got chopped into a million pieces. It’s like trying to watch a movie when someone keeps pausing it every 60 seconds—incredibly frustrating, and you definitely don’t get the full experience. Your body never gets that deep, restorative sleep it desperately needs, which explains why you feel like garbage in the morning.
The Three Types of Sleep Apnea You Should Know
So when I went to my first appointment, I just assumed all sleep apnea was the same. Boy, was I wrong. There’s actually three different types, and understanding which one you have is pretty important for figuring out the best treatment.
Obstructive Sleep Apnea (OSA) is the most common one—like, way more common than the other two. This is what I have, and it happens when your throat muscles relax too much during sleep. Basically, the soft tissue in the back of your throat collapses and blocks your airway. Think of it like a garden hose that gets kinked—the water (or in this case, air) can’t get through properly. Risk factors include being overweight, having a thick neck, or just having a naturally narrow airway. I checked all those boxes, unfortunately.
Central Sleep Apnea (CSA) is a whole different beast. This is when your brain temporarily forgets to send the signal to your breathing muscles. It’s not a physical blockage—it’s more like a communication error between your brain and your body. This type is less common and is often related to other medical conditions like heart failure or stroke. My uncle actually has this type after his heart attack, and his treatment looks pretty different from mine.
Then there’s Complex Sleep Apnea Syndrome, which doctors sometimes call treatment-emergent central sleep apnea. This one’s kind of a double whammy—you start with obstructive sleep apnea, but when you begin CPAP treatment, central sleep apnea symptoms pop up too. It’s like your body saying, “Oh, you thought you had it figured out? Think again!” Thankfully, this is the rarest type, and there are specialized treatments for it.
Knowing which type you have matters because the treatments can be really different. What works great for obstructive sleep apnea might not touch central sleep apnea at all.
Common Sleep Apnea Symptoms (And Why I Ignored Mine for Years)
Man, looking back, I can’t believe how many red flags I just completely brushed off. But I wasn’t alone in this—tons of people ignore these symptoms for years because they develop so gradually that they start to feel normal.
The biggest one is loud, chronic snoring that sounds like a freight train. My wife used to record me on her phone, and I sounded like I was choking on a kazoo. Not cute. But here’s the thing—not everyone who snores has sleep apnea, and not everyone with sleep apnea snores loudly. I had a buddy who barely snored at all but still had moderate sleep apnea. Go figure.
Gasping or choking during sleep is the scarier symptom. This usually wakes your bed partner up more than it wakes you up. My wife described it as me stopping breathing for what felt like forever, then suddenly gasping like I’d been underwater. That’s your body’s emergency response kicking in.
Here’s the symptom that finally made me get checked out: excessive daytime sleepiness. I’m talking about nodding off during meetings, fighting to keep your eyes open during your morning commute, needing a nap every single afternoon. I once fell asleep at a red light. That was my wake-up call, ironically.
Morning headaches were another big one for me. I’d wake up with this dull, throbbing headache that felt like a hangover, except I hadn’t touched a drop of alcohol. These happen because your oxygen levels are dropping during the night, and your blood vessels respond by dilating, which triggers pain.
The difficulty concentrating and memory problems sneaked up on me. I started forgetting conversations I’d had the day before, losing my train of thought mid-sentence, and just generally feeling like my brain was wrapped in cotton. My job performance was taking a hit, and I thought I was just getting old. Nope—my brain literally wasn’t getting enough oxygen at night to function properly during the day.
Mood changes and irritability are huge red flags too. I became this grumpy, short-tempered version of myself. Small things would set me off, and I was constantly anxious and on edge. Depression is actually really common with untreated sleep apnea, which makes sense when you’re exhausted and oxygen-deprived all the time.
Other symptoms include night sweats (I’d wake up drenched), frequent nighttime urination (up three or four times a night), and dry mouth or sore throat in the morning. If you’re checking off multiple boxes here, seriously, go talk to a doctor. Don’t wait five years like I did.

What Actually Causes Sleep Apnea?
So what makes some people develop sleep apnea while others sleep like babies their whole lives? Turns out, there’s a bunch of different factors at play, and for most people, it’s a combination of things rather than just one cause.
Excess weight is probably the biggest risk factor for obstructive sleep apnea. When you carry extra weight, especially around your neck and upper body, it puts pressure on your airway. Fat deposits around your upper airway can obstruct your breathing when you’re lying down. I’d gained about 40 pounds over ten years, and my neck had gone from a size 15 to a size 17 collar. That extra tissue was literally squeezing my airway shut at night. Fun times.
But here’s something that surprised me: you don’t have to be overweight to have sleep apnea. Some people just have naturally narrow airways or structural issues. Maybe your tonsils are enlarged, or you’ve got a deviated septum, or your jaw is positioned in a way that crowds your airway. One of my coworkers is thin as a rail but has sleep apnea because of his jaw structure.
Age plays a role too. Sleep apnea becomes more common as you get older because your throat muscles naturally lose some of their tone over time. It’s like everything else in your body—things start to sag a bit. Middle-aged and older adults are at higher risk.
Gender matters, though not as much as we used to think. Men are two to three times more likely to have sleep apnea than premenopausal women. But once women hit menopause, their risk goes way up. Something about hormones helps protect women until that point.
Lifestyle factors can make a huge difference. Alcohol consumption relaxes the muscles in your throat, making airway obstruction more likely. I used to have a couple of beers most nights, and cutting that out actually helped with my symptoms. Smoking irritates and inflames the upper airway, and certain medications like sedatives and tranquilizers can relax your throat muscles too much.
Family history is another piece of the puzzle. If your parents or siblings have sleep apnea, you’re at higher risk. There’s definitely a genetic component, whether it’s inherited physical characteristics or predisposition to the condition. My dad snored like crazy his whole life and probably had undiagnosed sleep apnea.
Finally, certain medical conditions increase your risk. Things like high blood pressure, type 2 diabetes, Parkinson’s disease, polycystic ovary syndrome, and hormonal disorders can all contribute. It’s like a domino effect—one condition makes another more likely.
How Sleep Apnea Affects Your Body (The Scary Stuff)
Okay, this is the section that honestly scared me straight when I finally learned about it. Sleep apnea isn’t just about being tired—it can seriously mess up your entire body if you leave it untreated.
The cardiovascular effects are no joke. Every time your breathing stops and your oxygen levels drop, it stresses your cardiovascular system. Your blood pressure spikes, your heart rate becomes irregular, and over time, this repeated stress can lead to high blood pressure, heart disease, heart attacks, and strokes. My doctor told me that people with severe untreated sleep apnea are four times more likely to have a stroke. That got my attention real fast.
I already had borderline high blood pressure before my diagnosis, and it was getting worse every year despite medication. Within six months of treating my sleep apnea, my blood pressure improved so much I was able to reduce my medication. That connection between sleep apnea and hypertension is super strong.
The metabolic effects are equally concerning. Sleep apnea messes with your body’s ability to use insulin, which increases your risk of developing type 2 diabetes. Even if you don’t get full-blown diabetes, you might develop metabolic syndrome, which is a cluster of conditions that increase your risk for heart disease and stroke. I noticed I was gaining weight easier and having a harder time losing it, even though I wasn’t eating that differently. Turns out, sleep apnea was throwing my hormones and metabolism completely out of whack.
Mental health takes a massive hit too. Depression and anxiety are way more common in people with sleep apnea. When your brain isn’t getting enough oxygen and you’re not getting restorative sleep, your mental health suffers. I went through a really dark period where I felt hopeless and overwhelmed by everything. Getting my sleep apnea treated literally saved my mental health, and I’m not being dramatic.
The daytime functioning and safety risks are huge concerns. Excessive sleepiness makes you dangerous behind the wheel—people with untreated sleep apnea are up to five times more likely to have traffic accidents. I mentioned falling asleep at that red light earlier. I’m lucky it was just a red light and not while I was moving. People with sleep apnea also have higher rates of workplace accidents and injuries.
Your cognitive function deteriorates too. Memory, concentration, decision-making, reaction time—all of it gets worse. I felt like I’d lost 20 IQ points. Simple tasks took forever, and I’d make stupid mistakes I never would have made before.
The longer you let sleep apnea go untreated, the worse these effects become. It’s progressive. This stuff really motivated me to stick with my treatment, even when wearing a CPAP mask felt awkward and uncomfortable.
Getting Diagnosed: What to Expect
So you think you might have sleep apnea. Now what? Let me walk you through what the diagnosis process actually looks like, because I went into it totally clueless and anxious about the whole thing.
First, when should you see a doctor? If you’re experiencing loud snoring, daytime sleepiness that interferes with your life, witnessed breathing pauses during sleep, or you’re waking up gasping or choking, it’s time to make an appointment. Don’t wait for it to get worse. I wish I’d gone in after the first year instead of the fifth. Start with your primary care doctor—they can refer you to a sleep specialist if needed.
The initial consultation involves a lot of questions. They’ll ask about your sleep habits, symptoms, medical history, medications, and lifestyle. Be honest about everything, including alcohol use and any substances you’re taking. They’ll examine your neck, throat, and mouth, and might measure your neck circumference. (Mine was 17.5 inches, which is above the risk threshold of 17 inches for men.)
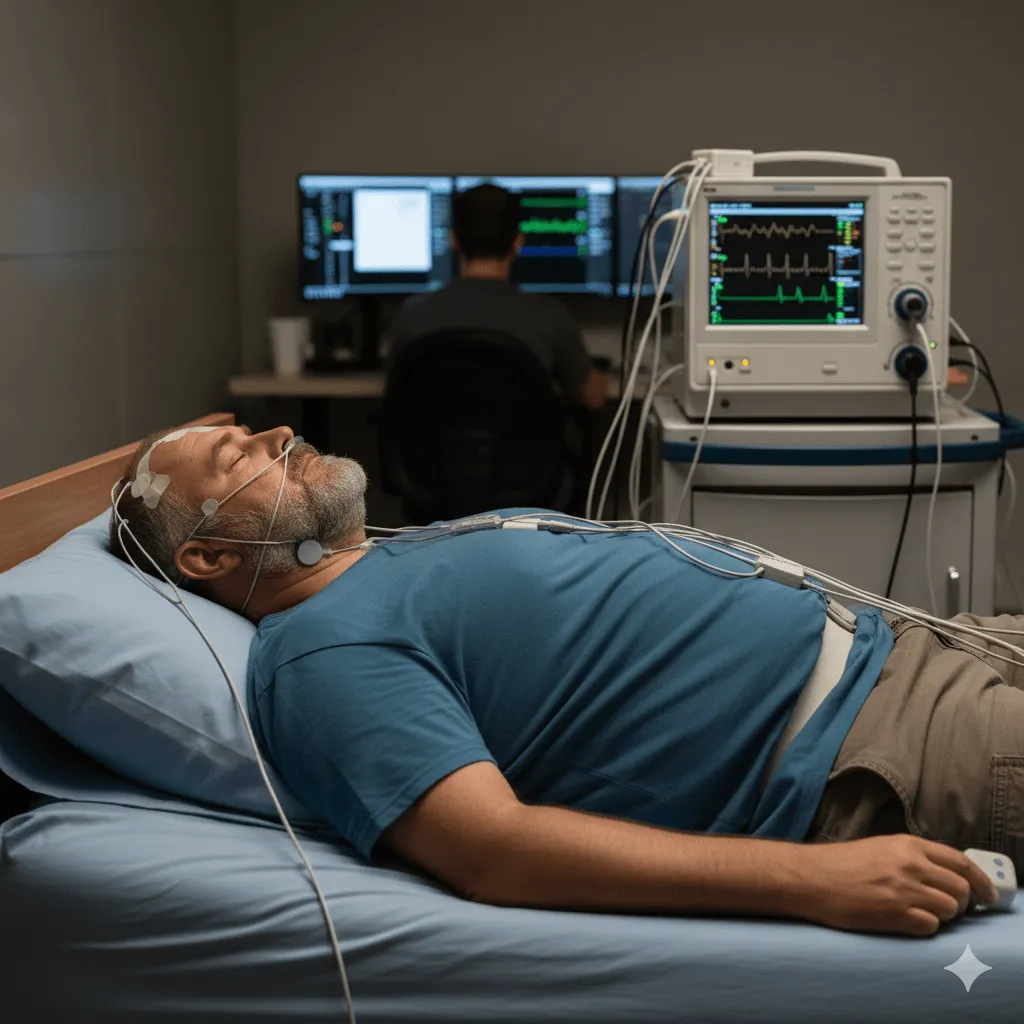
Then comes the sleep study, which is the gold standard for diagnosing sleep apnea. There are two types: in-lab polysomnography and home sleep tests.
In-lab sleep studies (polysomnography) are what I did. You spend the night at a sleep center where they hook you up to a bunch of monitors. Yeah, it sounds intimidating, but it wasn’t as bad as I thought. They monitor your brain waves, eye movements, heart rate, breathing patterns, oxygen levels, and body movements. You’ve got wires and sensors all over you, which feels weird at first, but I actually managed to fall asleep. The technicians are watching everything remotely, so if you need help or have to use the bathroom, they can assist you.
I’m not gonna lie—sleeping in a strange bed with all that equipment on was awkward. But the data they collected was incredibly detailed and showed exactly what was happening during my sleep. My results showed 47 apnea events per hour, which classified me as having severe obstructive sleep apnea. That number was sobering.
Home sleep tests are another option and are becoming more common. They’re less comprehensive but way more convenient. You pick up a portable monitoring device from your doctor’s office, use it at home for one or more nights, and return it for analysis. These tests typically monitor your breathing, oxygen levels, and heart rate, but they don’t measure brain activity or sleep stages. They’re usually used for people who clearly have sleep apnea and don’t have complicated medical issues.
What doctors look for in results is something called the Apnea-Hypopnea Index (AHI), which measures how many times per hour your breathing stops (apnea) or becomes very shallow (hypopnea). An AHI of 5-14 is mild, 15-29 is moderate, and 30 or more is severe. They also look at your oxygen saturation levels and how fragmented your sleep is.
Getting diagnosed was honestly a relief for me. Finally, there was an explanation for why I’d felt so terrible for so long. It wasn’t just me getting old or being lazy—there was an actual medical condition that could be treated.

Treatment Options That Actually Work
Alright, here’s where things get practical. Once you’re diagnosed, you’ve got options. Some work better than others depending on your specific situation, and what works for someone else might not be the best for you.
CPAP therapy (continuous positive airway pressure) is the most common and most effective treatment for moderate to severe obstructive sleep apnea. This is what I use, and I’m not gonna sugarcoat it—there’s an adjustment period. A CPAP machine gently blows air into your throat through a mask you wear over your nose or nose and mouth. The constant air pressure keeps your airway open so it can’t collapse.
My first few weeks with CPAP were rough. The mask felt claustrophobic, the air pressure seemed too strong, and I kept ripping the mask off in my sleep. But I stuck with it, and by week three, something clicked. I started waking up actually refreshed. The daytime sleepiness started fading. It was like someone had been slowly turning down the volume on my life for years, and suddenly everything got turned back up to full volume. Colors seemed brighter, food tasted better, I had energy again.
The key with CPAP is finding the right mask fit and pressure settings. Don’t give up if the first mask doesn’t work—there are tons of different styles. Work with your equipment provider to try different options. And use it every single night, even for naps. Consistency is everything.
Oral appliances are another option, especially for mild to moderate sleep apnea or for people who can’t tolerate CPAP. These are custom-fitted devices that look kind of like sports mouthguards. They work by repositioning your lower jaw and tongue to keep your airway open. My dentist offered me one initially, but with my severe apnea, CPAP was the better choice. One of my friends uses an oral appliance though, and he loves it—way less bulky than CPAP equipment, easier for travel.
Lifestyle changes can make a real difference, especially for mild cases. Weight loss is huge if you’re overweight. Losing even 10-15% of your body weight can significantly reduce apnea symptoms. I’ve lost about 25 pounds since my diagnosis (with 15 more to go), and my AHI has dropped from 47 to around 8 with CPAP. My doctor thinks if I lose more weight, I might be able to eventually stop using the machine, though that’s not guaranteed.
Avoiding alcohol and sedatives, especially before bedtime, helps because they relax your throat muscles. Quitting smoking reduces inflammation in your airway. These changes won’t cure sleep apnea by themselves, but they definitely help.
Positional therapy works for some people whose apnea is worse when sleeping on their back. Special pillows or devices can train you to sleep on your side. I tried taping a tennis ball to the back of my pajamas, which is an old-school trick to prevent back-sleeping. It sorta worked, but I still needed CPAP.
Surgery is an option for certain cases, usually when there’s a clear anatomic problem or when other treatments have failed. Procedures can include removing excess tissue from your throat, repositioning your jaw, or implanting a device that stimulates the nerve controlling your tongue (Inspire therapy). Surgery’s not a guaranteed fix and comes with risks, so it’s usually considered after less invasive options haven’t worked.
There are also alternative treatments like throat exercises (myofunctional therapy) that can strengthen the muscles in your airways. The evidence on these is mixed, but some people swear by them as a supplement to other treatments.
The bottom line? Treatment exists, it works, and it can genuinely change your life. Don’t suffer in silence or give up after one bad experience with CPAP. Keep working with your healthcare team until you find what works for you.
Living with Sleep Apnea: Real Talk from Someone Who’s Been There
Let’s get real about what it’s actually like living with sleep apnea and managing treatment long-term, because this is the stuff nobody really tells you about in the doctor’s office.
Adjusting to CPAP is probably the biggest hurdle. That first night, I looked at myself in the mirror wearing my mask and thought, “This is what my life has become?” It’s not sexy, it’s not comfortable at first, and you feel like Darth Vader. My wife had to get used to it too—sleeping next to someone hooked up to a machine takes some adjustment.
But here’s what I learned: modern CPAP machines are way quieter than older models. Mine makes less noise than a fan. Most of the sound comes from air leaks around the mask, which usually means it doesn’t fit right. Getting the fit dialed in is crucial. I went through three different mask styles before finding one that worked for me.
Some practical CPAP tips nobody told me: use distilled water in the humidifier, clean your equipment weekly, replace filters regularly, and gradually increase your air pressure if it feels too strong. Starting with the “ramp” feature—where the machine starts at lower pressure and gradually increases—helped me fall asleep easier. And yeah, you’ll probably still mouth-breathe sometimes even with a nasal mask, which can cause dry mouth. I keep water on my nightstand and use a chinstrap on particularly dry nights.
Making lifestyle changes stick is the other major challenge. It’s easy to say “lose weight and exercise more,” but when you’re exhausted from years of poor sleep, finding the motivation is hard. I started small—just walking 15 minutes after dinner. Once my sleep improved with CPAP treatment, I had more energy to do more. It became a positive cycle instead of a vicious one.
I had to have some tough conversations with myself about my drinking habits too. I wasn’t an alcoholic or anything, but those couple of beers every night were definitely making my apnea worse. Cutting back to weekends only made a noticeable difference.
Working with your healthcare team is ongoing. I have follow-up appointments every six months where they download data from my CPAP machine and adjust things if needed. At first I felt embarrassed about the nights when my usage sucked—like I was failing somehow. But my sleep doctor reminded me this is medical treatment, not a moral judgment. Some nights are just harder than others.
The impact on relationships is real. Sleep apnea and its treatment affect your partner too. My wife was relieved when I finally got treated—she’d been worried about me for years and hadn’t been sleeping well herself because of my snoring and gasping. But she also had to adjust to the noise of the machine, my earlier bedtime (because I needed a strict sleep schedule), and the fact that spontaneous intimacy got a bit more complicated. We figured it out, and honestly, our relationship improved because I wasn’t an exhausted grump anymore.
Traveling with CPAP seemed daunting at first, but it’s become routine. My machine fits in a small carry-on bag, and most airlines don’t count it toward your bag limit. I bring my own extension cord because hotel outlets are never where you need them. The key is to plan ahead and not let travel be an excuse to skip treatment.
Some nights I still struggle with motivation to put the mask on. When I’m sick or stressed, sometimes I just want to sleep “normally.” But then I remember how terrible I felt before treatment, and I strap that mask on. One bad night of breathing won’t kill you, but patterns of non-compliance will bring all those old problems back.
The biggest thing living with sleep apnea taught me is that treating chronic conditions requires persistence and self-compassion. You’re gonna have setbacks. You’re gonna have nights where you rip the mask off at 3 AM. You’re gonna skip cleaning your equipment sometimes. That’s being human. What matters is getting back on track and not giving up.

Conclusion
Look, if you’ve made it this far through this article, you clearly care about understanding sleep apnea—whether for yourself or someone you love. And that matters, because awareness is honestly the first step toward getting help.
Sleep apnea is way more than just snoring or feeling tired. It’s a serious medical condition that affects millions of people and can have major consequences for your physical health, mental wellbeing, and quality of life. But here’s the hopeful part: it’s also highly treatable. With the right diagnosis and treatment plan, most people see dramatic improvements.
If you’re experiencing symptoms—the excessive daytime sleepiness, the loud snoring, the morning headaches, the mood changes—please don’t brush them off like I did for years. Make an appointment with your doctor. Get a sleep study. Figure out what’s going on. The temporary discomfort of diagnosis and initial treatment is nothing compared to the long-term relief and improved health you’ll experience.
And if you’ve already been diagnosed but you’re struggling with treatment compliance, know that you’re not alone. Millions of us are out there every night strapping on our CPAP masks or using our oral appliances. It gets easier. Your health is worth the adjustment period.
Remember that everyone’s situation is different. What works for me might not work for you, and that’s okay. Work with your healthcare team to customize your treatment based on your specific needs, lifestyle, and preferences. Don’t give up if the first approach doesn’t work—there are options.
Finally, if you’re reading this because you’re worried about a partner or family member who has symptoms, encourage them gently to get checked out. Share what you’ve learned. Offer to go with them to appointments. Sometimes having that support makes all the difference.
I’d love to hear from you in the comments! Are you dealing with sleep apnea? What’s been your experience with treatment? What tips would you share with someone newly diagnosed? Let’s build a community where we can support each other through this journey. Your experience might be exactly what someone else needs to hear today.
Sweet dreams, everyone—and may they actually be restful ones!


